A word about the title. To be as inclusive as possible, this toolkit was NOT titled “Recognizing Females on the Autism Spectrum” as that could preclude a significant number of individuals who do not adhere to or identify with a binary gender.
Intended audience:
This toolkit is designed to sensitize educators, health care professionals as well as parents to the potential presence of autism in females, non-cisgendered males, as well as those who do not identify with a binary gender.
Objectives for the reader:
- To understand that the gender ratio of 3-4.3 males to 1 female is a relic of the initial description of autism
- To understand that multiple biases are at play to maintain a higher number of diagnosed males than non-males
- To realize that the classification system, diagnostic tools, as well as research have all promoted the male phenotype of autism
- To become familiar with the differences in presentation between autistic males and females
- To actively seek to identify females, non-cisgendered males, transgendered as well as those who do not identify with a binary gender, so that they can receive appropriate supports
- To understand the multitude of obstacles to female diagnoses
“Evidence that clinicians are missing girls with autism has been building for years. Because autistic girls tend to exhibit different traits than autistic boys do, they are frequently overlooked by teachers, doctors and standard diagnostic tools. Those omissions carry over into the research literature, where studies typically include three to six males for every female",
says William Mandy, a clinical psychologist at University College London.
 | Autism Spectrum Conditions (ASC) are all too often missed or identified late in females; subsequently these women are mislabeled or overlooked completely.1 We know they exist. In epidemiological studies the gender ratio is 2-3 males for every female. 2,3,4 Adult diagnostic clinics reveal a low ratio as well; in these clinics there are 2 males to 1 female.5 Mattila and her colleagues6claim that the ratio could fall to 1.8 males to every one female. |
Gender ratios
The ratio of 3/1- 4.3/1 males to females7 reflects the accepted ratio since the initial observation of the known condition. It was not questioned but rather was so deeply entrenched that it has been accepted as fact. But this ratio should not have been immortalized without being questioned and critiqued. Hartung and Widiger8 assert that if a gender is known to be predominant (which in autism we know it is), regardless of pathology, it is only responsible to explore the potential for bias in either the sampling or the diagnosis. Better late than never.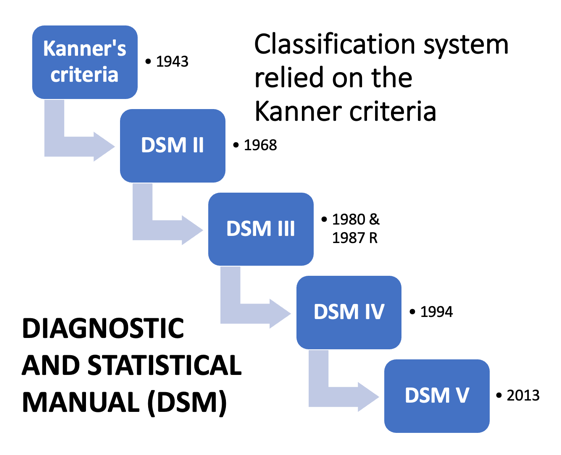
Why are females overlooked or diagnosed late?
Autism has been thought of as a male condition since the seminal work of Kanner9 and Asperger.10 Both men identified autism in boys, and only later did Asperger relax that attitude and acknowledge that girls too could be autistic. Their characterization of the condition was then reflected in the classification system known as the Diagnostic and Statistical Manual (DSM).11
Diagnostic tools were developed that meshed with the DSM criteria for autism. For instance, upon direct examination,12 the ADI-R (Autism Diagnostic Interview-Revised)13 and the ADOS-G (Autism Diagnostic Observation Scale – Generic)14 related well to the DSM-IV-TR (Diagnostic and Statistical Manual, 4th edition, text revision).11 So, with great intention diagnostic tools perpetuated the criteria in the classification system which stemmed from Kanner and Asperger, further reinforcing that primarily males receive a diagnosis of autism. 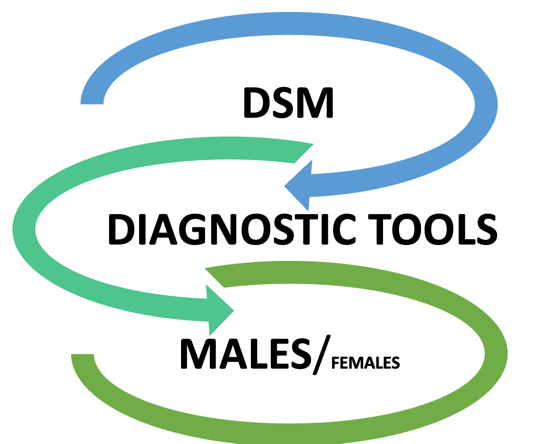
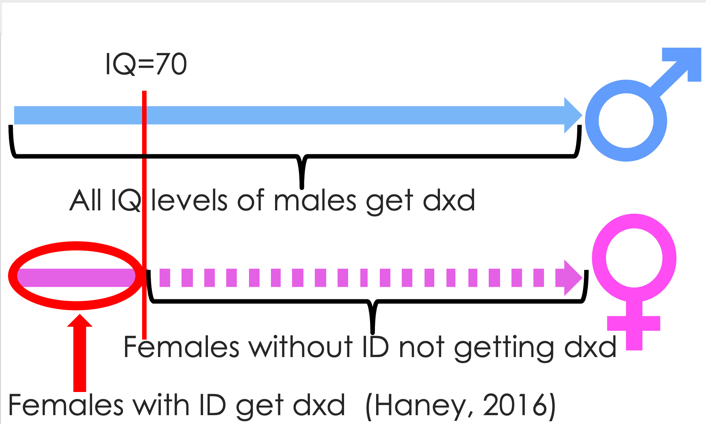
The way the diagnostic tools are currently designed, they lean to diagnosing the typical male ASC presentation.15 They do not take into account the variability of autistic symptoms by gender.16 If females present symptoms not included in the diagnostic algorithms for tools like the ADI-R, then of course a diagnosis of autism cannot be made.17 Looking specifically at the ADI-R, (as it, in conjunction with the ADOS, are considered the ‘gold standard’)18 there are 4 items that are crucial to the diagnostic algorithm, and they differentiate males and females.16 The endorsement that the item is an ‘issue’ for the individual loads toward identification of autism, however, these four items are insensitive to females without intellectual disability,19 and that is where we get the discrepancies in autism between males/females and females with/without intellectual disability (dotted line).
The ADOS, too, has challenges when it comes to identifying females as it relies on observation. As most autistic females are adept at masking, the ADOS is insensitive to identifying females.16 20
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
Most of what we know about autistic females has been gathered from females who have met the male phenotype for autism,21 in other words, females who have been diagnosed using the existing classification system and subsequent diagnostic tools, which we know have a male bias.15
Hartung and Widiger 8 warned of sampling bias as well when one gender dominates a specific condition. Sampling bias does exist. In a meta-analysis of 392 articles on autism, 80% of the study participants were male.22
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |

Clinicians and educators are looking for males in the belief that autism is a male condition. Males generally present with more overt autistic traits. 23, 24, 25, 26, 27, 28 As males tend to be externalizers; they may present as more disruptive in a school environment.21 Females may be less likely to have externalizing behaviours (hyperactivity/impulsivity and conduct problems), and instead are more likely to have internalizing problems like anxiety, depression and eating disorders.29, 30
“If the expression of symptoms of a disorder differ by gender, the development of diagnostic criteria will be biased toward the gender that externalizes psychic distress and exhibits socially unacceptable behavior” 8
Teachers may fail to recognize ‘autistic females’ too. They have fewer concerns about the behavior of girls30 and even when clinicians recognize social/communication deficits, teachers fail to recognize this.21 For example, in a study of playground behaviour, Dean and colleagues31 found that autistic boys were more likely to stand out as ‘loners’ among their peers. Girls, however, may bounce from social group to social group and flit about like the proverbial social butterfly which, to the onlooker, makes them appear to be socially confident and competent, when in fact they may be shifting groups because of rejection.
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |
| Belief that it’s a ‘male condition’ |
Autistic traits: quantity/severity and type
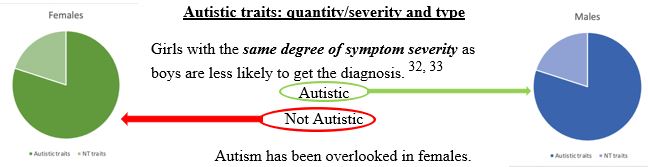
Repetitive and restricted behaviours and interests (RRBIs)

Much is made of RRBIs. They are included in the DSM classification system.21 They are an integral component of diagnostic tools.16, 17 Many people think of RRBIs as THE indicator of autism, and females have RRBIs, but they have fewer RRBIs than males34, 35, 36, 37, 38 and their special interests are not that SPECIAL.
Females have circumscribed interests, even intense interests, but they do not differ SO greatly from their neurotypical peers.39 Ponies, boy bands, animals, fashion, makeup, nail polish can all be transfixing for the autistic female, but as a focused interest they do not make her stand out as appreciably odd.Furthermore, females engage in fewer rituals than males, and take less interest in ‘part of objects’ (e.g., spinning wheels on a toy car).14This poses a problem for securing a diagnosis because the DSM and diagnostic tools all emphasize RRBIs; and males may be more likely to endorse this distinction in dramatic fashion while females may not.
Camouflage, masking, adaptive morphing
“Is the discrepancy between the person’s ‘external’ behavioural presentation in social–interpersonal contexts and the person’s ‘internal’ status (i.e., dispositional traits and/or social cognitive capability).” 40
Camouflaging, masking, or adaptive morphing are when a person acts in a way that they believe people want them to be. It can include, for example matching voice, accents, adopting a hairstyle, a gait, a style. It can be making eye contact, even though it causes discomfort, or controlling self-stims when in unaccepting company. This can also include rehearsing before an event; self-reminders to sit up straight, to not pick at teeth or twirl hair, or the practicing of filler statements. Much effort goes into this behaviour. They observe, and analyze, then they adopt that which they believe to be acceptable to society. 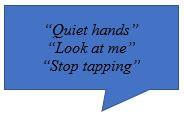
How have we contributed to masking? How do we reinforce masking behaviours?
Camouflaging is experienced as an obligation rather than a choice.40
Autistic females are more likely than males to camouflage; 90% of females have engaged in camouflaging42, 41 This behaviour reduces the observability of autistic traits, which may make it harder to identify autism in female-presenting people.43, 44, 30
Some autistic people credit camouflaging for their social and vocational successes, as they experience less stigma and marginalization in these spaces when their autistic traits are less pronounced. Unfortunately, camouflaging is seriously exhausting and can take a serious toll on mental health with depression and anxiety, to the point where masking is a risk marker for suicidality. 43, 42 Camouflaging can prevent or seriously delay an autism diagnosis, further reinforcing the gender differences in diagnosis. 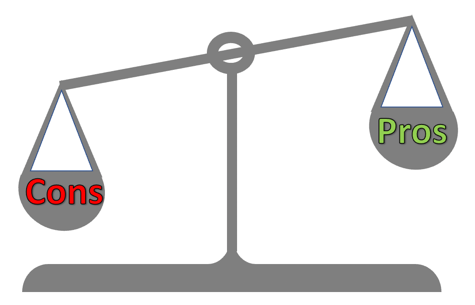

Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |
| Belief that it’s a ‘male condition’ |
| Stigma and marginalization can lead to camouflaging autistic traits |
When another condition is SO OBSERVABLE, the ASC may be less salient,
For example, in the case of eating disorders
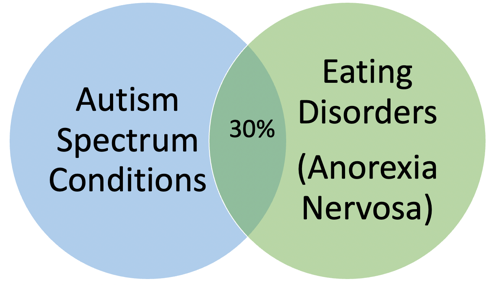
Autism and Eating Disorders
Autistic females may also be present in higher numbers than recognized in eating disorder (ED) clinics. Many females who receive treatment for an ED also present with autistic characteristics.45 Their ED may be their most conspicuous area of need insofar as it threatens their physical wellbeing. In the presence of a potentially debilitating physical condition, autistic traits may be overlooked or may not be prioritized for identification. Females with ED in the Babb et al. study45 who also had autistic traits tended to be erroneously labeled ‘resistant’ and ‘naughty’; many of these women knew their symptoms were not associated with the ED.
There is a significant overlap between autism and eating disorders (ED).29, 46, 47 For example, the prevalence of ASC in persons diagnosed with anorexia nervosa is 30%.48 Clinic patients with both anorexia nervosa and ASC fail to respond to treatment like those who are not comorbid for ASC. Those with ASC have worse adaptive functioning, and they require more intensive and longer treatment regimens.49 It is therefore critical to make the distinction between those with and without ASC to provide the most appropriate intervention regimen.
“When I was in hospital, I kept getting told off for walking on tip toes and for fidgeting a lot…they thought I was doing these things to burn more calories, except I’d been doing them for as long as I could remember” 45(AW09-ED but pre-ASC)
“For example, she would want to put a pea on each of the prongs of the fork, but [staff] said ‘oh no you can’t be doing that, you shouldn’t be doing that’ and corrected her when she was doing it, because they thought it was being driven by the eating disorder.” 45 (HCP03 regarding patient with ED but pre-ASC)
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |
| Belief that it’s a ‘male condition’ |
| Stigma and marginalization can lead to camouflaging autistic traits |
| An ED may be disguising their ASC |
When another condition is SO OBSERVABLE, the ASC may be less salient,
For example, in the case of sexual and gender minorities (SGM)
Autism and SGM
- ◦SAB – sex assigned at birth
- ◦AFAB – assigned female at birth
- ◦AMAB – assigned male at birth
- ◦Gender identity – one’s concept of self
- ◦Gender diverse – all who do not identify with SAB
- ◦Gender minority – when gender identity does not match sex assigned at birth
- ◦Sexual orientation – one’s romantic/sexual attraction
- ◦SGM – sexual and gender minority
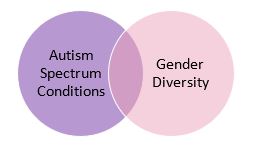
Autistics are more likely than neurotypicals to be gender diverse, and gender diverse folks are more likely to be autistic than are cisgender people50, 51
In gender diverse children, the rate of ASC is approximately 37 times higher than would be expected in the general population.52, 53, 54 Levels of autistic traits and ASC were higher for AFAB than AMAB54, 55 In addition, ASCs are far higher in the transgender group than in the general population; 22.5% of transgender adolescents and adults had a diagnosis of autism.50
When autistics are assessed for SGM status, 15% identified as gender diverse (percentage higher for AFAB) in comparison to fewer than 5% of the general population identifying as gender diverse.56 Rates of transgender identity in autistics is 20 to 40 times higher than population estimates.57 Perhaps the transgender presentation disguises the autism. When a parent has a teenager who discloses or acts upon their identity as differing from the sex which was assigned at birth, THAT will probably garner the parent’s attention far more than the fact that the child is struggling socially. Furthermore, they would have a ‘perfect’ excuse for why they are struggling socially; the salient presentation will be thought to be responsible.
Just as eating disorders clinics may open the door to the identification of female autistics, so may gender identity clinics.
Sexual orientation plays a role in identifying ‘would be autistics’ as well. Only 30% of autistics claimed to be heterosexual in comparison to 70% of neurotypicals.56 Autistic females present with greater diversity in their sexuality than either their male autistic counterparts or neurotypical female peers; they are less likely to be heterosexual than either group.58 Hence, the most salient, or noticeable presentation of a pre-adolescent, for example, may be an unexpected sexual orientation.
To date there has been no speculation regarding the appropriateness of applying that which are thought to be ‘female characteristics’ of autism, to men, gay men specifically, but let me be the first.
When presenting a ‘female autism identification’ talk at ASHA (American Speech and Hearing Association) in Boston in 2018, a gay man in the audience found the ‘female characteristics’ applied to him completely; whereas, he had dismissed the characteristics of the male autistic phenotype as found he did not resonate to them.
Personal experience – Glenis Benson, PhD
Do we need a continuum of autistic characteristics to find applicability across all, regardless of gender?
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |
| Belief that it’s a ‘male condition’ |
| Stigma and marginalization can lead to camouflaging autistic traits |
| An ED may be disguising their ASC |
| Gender diversity, and sexual orientation may be disguising their ASC |
Social and communication abilities
Females with ASC demonstrate relative strengths in socio-communicative abilities compared to males with ASC.60 They are better than males at non-verbal communication strategies and gestural use,36 and better at reciprocal conversations.21 Females are simply more socially motivated and have a greater capacity for traditional friendships.59, 60 When you add their ability to imitate, to camouflage and to mimic, to their increased motivation for social interaction, the presentation proves to be a great disguise for their autistic traits. They can hide in plain sight; they do not stand out socially to the same degree as their male counterparts because they can fake it so well. By adolescence, camouflaging and overexerting oneself socially can become mentally and emotionally exhausting, and it can impact other areas of life including mental health and functioning.61
Girls are ambiguous in their presentation. They are not as noticeable as clinicians would expect for ‘typical’ ASC impairment.21
Obstacles to female diagnoses | |
| Bias in diagnostic criteria/diagnostic tools |
| Biased sampling in research |
| Belief that it’s a ‘male condition’ |
| Stigma and marginalization can lead to camouflaging autistic traits |
| An ED may be disguising their ASC |
| Gender diversity, and sexual orientation may be disguising their ASC |
| Social communication skills, though superficial, allow them to fly under the radar |
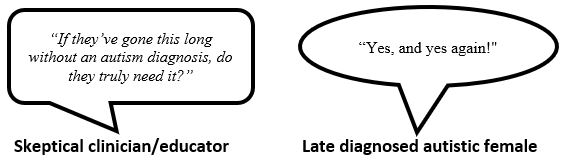
The cost of misidentification, late identification, and no identification
Given brain plasticity, the earlier intervention occurs, the better.37 It is not as though these females avoid life struggles; they endure relationship as well as academic struggles in addition to the internalized problems of anxiety and depression, among others.43, 62, 42 They are misidentified, over-medicated63 and many are hospitalized for eating disorders.47 They experience both burnout and exhaustion; camouflaging is exhausting.43, 42 Given the adoption of an alternate identity, they are left questioning what about them is authentic and what is the mask.64 Because they have learned to socialize superficially, they do not accurately read non-verbal or subtle verbal signals making them vulnerable to sexual exploitation and abuse.43 In addition, autistic females are 13 times more likely to die by suicide than non-autistics.65, 66 These females are being failed by the system. By not being accurately diagnosed they do not receive autism-specific intervention or supports that could enhance their well-being and quality of life. We need to do better.
Autistic females have been overlooked not just by society but by science 67
Next Steps
Professional development for health care professionals as well as educators is critical. They all need to be trained on the various presentations of autism, including the intersection of gender and age43, 68, 5 | ||||
Clinics need to be broad in their scope. Child development clinics need to be sensitive to the potential for ASC across all genders, inclusive of those who present diversely. Eating Disorders Clinics and Gender Diversity Clinics need to be sensitized to the potential for ASC in those presenting with both ED and SGM, respectively. | ||||
Diagnostic methods need to be revamped and adjusted. Observational methods are contraindicated with the prevalence of masking.69 It is imperative to employ diagnostic tools and questionnaires that accurately measure traits in females as well as non-binary individuals.70 | ||||
| Some instruments that can be of assistance are: Q-ASC (Questionnaire for ASC)71 CAT-Q (Camouflaging Autistic Traits Questionnaire72 GABS (Gendered Autism Behavioral Scale)73 ASSQ-Rev (Autism Spectrum Screening Questionnaire74 | |||
Researchers need to be actively recruiting females and other non-cis-male study participants.40 These researchers can also seek guidance from adult female autistics on how to recruit more study participants who are female, trans, gender diverse, and non-binary.67 | ||||
Autism; it’s not just for males anymore.
References
1. Lai, M. C., Dr, & Baron-Cohen, S. (2015). Identifying the lost generation of adults with autism spectrum conditions. The Lancet. Psychiatry, 2(11), 1013–1027. https://doi.org/10.1016/S2215-0366(15)00277-1
2. Constantino, J. N., Zhang, Y., Frazier, T., Abbacchi, A. M., & Law, P. (2010). Sibling recurrence and the genetic epidemiology of autism. The American Journal of Psychiatry, 167(11), 1349–1356. doi:10.1176/appi.ajp.2010.09101470.
3. Kim YS, Leventhal BL, Koh Y-J, Fombonne E, Laska E, Lim E-C, et al. Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry. 2011;168(9):904–912. doi: 10.1176/appi.ajp.2011.10101532.
4. Zwaigenbaum, L., Bryson, S. E., Szatmari, P., Brian, J., Smith, I. M., Roberts, W., Vaillancourt, T. & Roncadin, C. (2012) ‘Sex differences in children with autism spectrum disorder identified within a high-risk infant cohort’. Journal of Autism and Developmental Disorders, 42(12), 2585–2596.
5. Rutherford, M., McKenzie, K., Johnson, T., Catchpole, C., O’Hare, A., McClure, I., et al. (2016). Gender ratio in a clinical population sample, age of diagnosis and duration of assessment in children and adults with autism spectrum disorder. Autism, 20(5), 628–634.
6. Mattila, M. L., M.D, Kielinen, M., Linna, Sirkka-Liisa, M.D., Jussila, Katja, M.A, Ebeling, Hanna, M.D., Bloigu, Risto, M.Sc, Joseph, R. M., & Moilanen, Irma, M.D. (2011). Autism Spectrum Disorders According to DSM-IV-TR and Comparison With DSM-5 Draft Criteria: An Epidemiological Study. Journal of the American Academy of Child and Adolescent Psychiatry, 50(6), 583–592.e11. https://doi.org/10.1016/j.jaac.2011.04.001
7. Loomes, R., Hull, L., Polmear, W., Locke, M., (2017). What is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 56(6), 466–474. https://doi.org/10.1016/j.jaac.2017.03.013
8. Hartung, C. M., & Widiger, T. A. (1998). Gender differences in the diagnosis of mental disorders: Conclusions and controversies of the DSM-IV. Psychological Bulletin, 123(3), 260–278. doi:10.1037/0033-2909.123.3.260
9. Kanner, L. (1943) ‘Autistic disturbances of affective contact’. Nervous Child, 2, 217–250.
10. Asperger, H. (1991). ‘“Autistic psychopathy” in childhood’ (trans. U. Frith). In U. Frith (ed.), Autism and Asperger Syndrome (pp. 37–92). Cambridge: Cambridge University Press.
11. American Psychiatric Association. (2013) Diagnostic and statistical manual of mental disorders (DSM-5). Arlington (VA): American Psychiatric Pub; 2013.
12. De Bildt, A., Sytema, S., Ketelaars, C., Kraijer, D., Mulder, E., Volkmar, F., & Minderaa, R. (2004). Interrelationship between autism diagnostic observation schedule-generic (ADOS-G), autism diagnostic interview-revised (ADI-R), and the diagnostic and statistical manual of mental disorders (DSM-IV-TR) classification in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders, 34(2), 129–137. https://doi.org/10.1023/B:JADD.0000022604.22374.5f
13. Lord C., Rutter M., & Couteur A.L. (1994). Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 24:659–85.
14. Lord C, Risi S, Lambrecht L, Cook EH, Leventhal, B. et al (2000). The ADOS-G (Autism Diagnostic Observation ScheduleGeneric): a standard measure of social-communication defcits associated with autism spectrum disorders. J Autism Dev Disord 30:205–223
15. Tubío-Fungueiriño, M., Cruz, S., Sampaio, A., Carracedo, A., & Fernández-Prieto, M. (2020). Social Camouflaging in Females with Autism Spectrum Disorder: A Systematic Review. Journal of Autism and Developmental Disorders, 51(7), 2190–2199. https://doi.org/10.1007/s10803-020-04695-x
16. Beggiato, A., Peyre, H., Maruani, A., Scheid, I., Rastam, M., Amsellem, F., Gillberg, C. I., Leboyer, M., Bourgeron, T., Gillberg, C., & Delorme, R. (2017). Gender differences in autism spectrum disorders: Divergence among specific core symptoms. Autism Research, 10(4), 680–689. https://doi.org/10.1002/aur.1715
17. Wilson, C.E., Murphy, C.M., McAlonan, G., et al. (2016). Does sex influence the diagnostic evaluation of autism spectrum disorder in adults? Autism Int J Res Pract 2016;20:808–19.
18. Kamp-Becker, I., Tauscher, J., Wolff, N., Küpper, C., Poustka, L., Roepke, S., Roessner, V., Heider, D., & Stroth, S. (2021). Is the Combination of ADOS and ADI-R Necessary to Classify ASD? Rethinking the “Gold Standard” in Diagnosing ASD. Frontiers in Psychiatry, 12, 727308–727308. https://doi.org/10.3389/fpsyt.2021.727308
19. Haney, J. L., (2016). Autism, females and the DSM-5: Gender bias in autism diagnosis. Social Work in Mental Health, 14(4), 396-407.
20. Lai MC, Lombardo MV, Pasco G, Ruigrok AN, Wheelwright SJ, Sadek SA, et al. A behavioral comparison of male and female adults with high functioning autism spectrum conditions. PLoS One 2011; 6: e20835.
21. Hiller, R.M., Young, R.L. & Weber, N. (2014) Sex Differences in Autism Spectrum Disorder based on DSM-5 Criteria: Evidence from Clinician and Teacher Reporting. J Abnormal Child Psychol (2014) 42:1381-1393.
22. Thompson, T., Caruso, M., & Ellerbeck, K. (2003). Sex matters in autism and other devel- opmental disabilities. Journal of Learning Disabilities, 7(4), 345–362.
23. Allison, C. (2018, July 1). Autistic Women & Nonbinary Network (AWN). Retrieved from http://awnnetwork.org/autistic-women-non-binary-network-awn/
24. Baron-Cohen S, Wheelwright S, Skinner R, Martin J, & Clubley E. (2001). The Autism- Spectrum Quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord 31(1):5–17
25. Constantino, J. & Todd, R. D. (2003). Autistic Traits in the General Population: A Twin Study. Archives of General Psychiatry, 60(5), 524–530. https://doi.org/10.1001/archpsyc.60.5.524
26. Posserud, M.-B., Lundervold, A. J., & Gillberg, C. (2006). Autistic features in a total population of 7-9-year-old children assessed by the ASSQ (Autism Spectrum Screening Questionnaire). Journal of Child Psychology and Psychiatry and Allied Disciplines, 47(2), 167–175. doi:10.1111/j.1469-7610.2005.01462.x.
27. Skuse, D. (2009). Is autism really a coherent syndrome in boys, or girls? The British Journal of Psychology, 100(1), 33–37. https://doi.org/10.1348/000712608X369459
28. Williams, J., Allison, C. Scott, F., Bolton, P., Baron-Cohen, S., Matthews, F., Brayne, C. (2008). The Childhood Autism Spectrum Test: Sex Differences. Journal of Autism and Developmental Disorders, 38, p. 1731-1739.
29. Huke, V., Turk, J., Saeidi, S., Kent, A., & Morgan, J. F. (2013). Autism spectrum disorders in eating disorder populations: A systematic review. European Eating Disorders Review: The Journal of the Eating Disorders Association, 21(5), 345–351. doi:10.1002/erv.2244.
30. Mandy, W., Chilvers, R., Chowdhury, U., Salter, G., Seigal, A., Skuse, D. (2012). Sex differences in autism spectrum disorder: evidence from a large sample of children and adolescents. J Autism Dev Disord. 2012;42: 1304-1313.
31. Dean, M., Harwood, R., & Kasari, C. (2017). The art of camouflage: Gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism: the International Journal of Research and Practice, 21(6), 678–689. https://doi.org/10.1177/1362361316671845
32. Dworzynski, K., Ronald, A., Bolton, P., & Happé, F. (2012). How different are girls and boys above and below the diagnostic threshold for autism spectrum disorders? Journal of the American Academy of Child and Adolescent Psychiatry, 51(8), 788–797. https://doi.org/10.1016/j.jaac.2012.05.018
33. Geelhand, P., Bernard, P., Klein, O., Van Tiel, B., & Kissine, M. (2019). The role of gender in the perception of autism symptom severity and future behavioral development. Molectular Autism, 10(1), 16.
34. Duvekot, J., van der Ende, J., Verhulst, F. C., Slappendel, G., van Daalen, E., Maras, A., & Greaves-Lord, K. (2017). Factors influencing the probability of a diagnosis of autism spectrum disorder in girls versus boys. Autism: the International Journal of Research and Practice, 21(6), 646–658. https://doi.org/10.1177/1362361316672178
35. Rubenstein, E., Wiggins, L. D., & Lee, L.-C. (2015). A Review of the Differences in Developmental, Psychiatric, and Medical Endophenotypes Between Males and Females with Autism Spectrum Disorder. Journal of Developmental and Physical Disabilities, 27(1), 119–139. https://doi.org/10.1007/s10882-014-9397-x
36. Rynkiewicz, A., Schuller, B., Marchi, E., Piana, S., Camurri, A., Lassalle, A., & Baron-Cohen, S. (2016). An investigation of the ‘female camouflage effect’ in autism using a computerized ADOS-2, and a test of sex/gender differences. Molecular Autism, 7(1), 10. doi:10.1186/s13229-016-0073-0.
37. Supekar, K., De los Angeles, C., Ryali, S., Cao, K., Ma, T., & Menon, V. (2022). Deep learning identifies robust gender differences in functional brain organization and their dissociable links to clinical symptoms in autism. The British Journal of Psychiatry, 1-8. doi:10.1192/bjp.2022.13
38. Tillmann, J., Ashwood, K., Absoud, M., Bölte, S., Bonnet-Brilhault, F., Buitelaar, J. K., et al. (2018). Evaluating sex and age differences in ADI-R and ADOS scores in a large European multi-site sample of individuals with autism spectrum disorder. Journal of Autism and Developmental Disorders, 1–16.
39. Young, H., Oreve, M.-J., & Speranza, M. (2018). Clinical characteristics and problems diagnosing autism spectrum disorder in girls. Archives de Pédiatrie : Organe Officiel de La Société Française de Pédiatrie, 25(6), 399–403. https://doi.org/10.1016/j.arcped.2018.06.008
40. Mandy, W. (2019). Social camouflaging in autism: Is it time to lose the mask? Autism: the International Journal of Research and Practice, 23(8), 1879–1881. https://doi.org/10.1177/1362361319878559
41. Lai, M.C., Lombardo, M. V., Ruigrok, A. N., Chakrabarti, B., Auyeung, B., Szatmari, P., Happé, F., & Baron-Cohen, S. (2017). Quantifying and exploring camouflaging in men and women with autism. Autism: The International Journal of Research and Practice, 21(6), 690–702. https://doi.org/10.1177/1362361316671012
42. Cassidy, S., Bradley, L., Shaw., & Baron-Cohen, S. (2018). Risk markers for suicidality in autistic adults. Molecular Autism, 9(1), 42.
43. Bargiela, S., Steward, R., & Mandy, W. (2016). The experiences of late-diagnosed women with autism spectrum conditions: An investigation of the female autism phenotype. Journal of Autism and Developmental Disorders, 46(10), 3281-3294.
44. Lai, M.C., Baron-Cohen, S., & Buxbaum, J. D. (2015). Understanding autism in the light of sex/gender. Molecular Autism, 6(1), 24–24. https://doi.org/10.1186/s13229-015-0021-4
45. Babb, C., Brede, J., Jones, C. R. G., Elliott, M., Zanker, C., Tchanturia, K., Serpell, L., Mandy, W., & Fox, J. R. E. (2021). ‘It’s not that they don’t want to access the support . . . it’s the impact of the autism’: The experience of eating disorder services from the perspective of autistic women, parents and healthcare professionals. Autism: The International Journal of Research and Practice, 25(5), 1409–1421. https://doi.org/10.1177/1362361321991257
46. Westwood H, Eisler I, Mandy W, et al. (2016). Using the autism-spectrum quotient to measure autistic traits in anorexia nervosa: a systematic review and meta-analysis. J Autism Dev Disord 2016;46(3):964–77.
47. Westwood, H., & Tchanturia, K. (2017). Autism Spectrum Disorder in Anorexia Nervosa: An Updated Literature Review. Current Psychiatry Reports, 19(7), 41–41. https://doi.org/10.1007/s11920-017-0791-9
48. Brown, C. & Stokes, M. A. (2020). Intersection of Eating Disorders and the Female Profile of Autism. Child and Adolescent Psychiatric Clinics of North America, 29(2), 409–417. https://doi.org/10.1016/j.chc.2019.11.002Carpenter, B., Happé, F., & Egerton, J. (2019). Girls and autism: educational, family and personal perspectives. Abingdon, Oxon; New York, NY: Routledge.
49. Tchanturia, K., Adamson, J., Leppanen, J., & Westwood, H. (2019). Characteristics of autism spectrum disorder in anorexia nervosa: A naturalistic study in an inpatient treatment programme. Autism: The International Journal of Research and Practice, 23(1), 123–130. https://doi.org/10.1177/1362361317722431
50. Strang, J. F., Janssen, A., Tishelman, A., Leibowitz, S. F., Kenworthy, L., McGuire, J. K., Edwards-Leeper, L., Mazefsky, C. A., Rofey, D., Bascom, J., Caplan, R., Gomez-Lobo, V., Berg, D., Zaks, Z., Wallace, G. L., Wimms, H., Pine-Twaddell, E., Shumer, D., Register-Brown, K., Sadikova, E., … Anthony, L. G. (2018). Revisiting the Link: Evidence of the Rates of Autism in Studies of Gender Diverse Individuals. Journal of the American Academy of Child and Adolescent Psychiatry, 57(11), 885–887. https://doi.org/10.1016/j.jaac.2018.04.023
51. Walsh, R. J., Krabbendam, L., Dewinter, J., & Begeer, S. (2018). Brief Report: Gender Identity Differences in Autistic Adults: Associations with Perceptual and Socio-cognitive Profiles. Journal of autism and developmental disorders, 48(12), 4070–4078. https://doi.org/10.1007/s10803-018-3702-y
52. de Vries, A.L.C., Noens, I.L.J., Cohen-Kettenis, P.T. et al. (2010). Autism Spectrum Disorders in Gender Dysphoric Children and Adolescents. J Autism Dev Disord 40, 930–936. https://doi.org/10.1007/s10803-010-0935-9
53. Jones, R. M., Wheelwright, S., Farrell, K., Martin, E., Green, R., Di Ceglie, D., & Baron-Cohen, S. (2011). Brief Report: Female-To-Male Transsexual People and Autistic Traits. Journal of Autism and Developmental Disorders, 42(2), 301–306. https://doi.org/10.1007/s10803-011-1227-8
54. Kung, K. T. F., (2020). Autistic traits, systemising, empathising, and theory of mind in transgender and non-binary adults. Molecular Autism, 11(1), 1–73. https://doi.org/10.1186/s13229-020-00378-7
55. Stagg, S. D., & Vincent, J. (2019). Autistic traits in individuals self-defining as transgender or nonbinary. European Psychiatry, 61, 17–22. https://doi.org/10.1016/j.eurpsy.2019.06.003
56. Kuyper, L., & Wijsen, C. (2014). Gender identities and gender dys- phoria in the Netherlands. Archives of Sexual Behavior, 43(2), 377–385.
57. George, R., & Stokes, M. A. (2018). Sexual Orientation in Autism Spectrum Disorder. Autism research: official journal of the International Society for Autism Research, 11(1), 133–141. https://doi.org/10.1002/aur.1892
58. Pecora, L.A., Hancock, G. I., Hooley, M., Demmer, D. H., Attwood, T., Mesibov, G. B., & Stokes, M. A. (2020). Gender identity, sexual orientation and adverse sexual experiences in autistic females. Molecular Autism, 11(1), 1–57. https://doi.org/10.1186/s13229-020-00363-0
59. Head, A. M., McGillivray, J. A., & Stokes, M. A. (2014). Gender differences in emotionality and sociability in children with autism spectrum disorders. Molecular autism, 5(1), 19. https://doi.org/10.1186/2040-2392-5-19
60. Sedgewick, F., Hill, V., Yates, R., Pickering, L., & Pellicano, E. (2016). Gender differences in the social motivation and friendship experiences of autistic and non-autistic adolescents. Journal of Autism and Developmental Disorders, 46, 1297–1306.
61. Mandy, W., Pellicano, L., St Pourcain, B., Skuse, D., & Heron, J. (2018). The development of autistic social traits across childhood and adolescence in males and females. Journal of Child Psychology and Psychiatry, 59(11), 1143–1151. https://doi.org/10.1111/jcpp.12913
62. Begeer, S., Mandell, D., Wijnker-Holmes, B., Venderbosch, S., Rem, D., Stekelenburg, F., & Koot, H. (2013). Sex Differences in the Timing of Identification Among Children and Adults with Autism Spectrum Disorders, Journal of Autism and Developmental Disorders, 43(5), 1151-1156.
63. Happé, F. “Autism as a Neurodevelopmental Disorder of Mind-Reading.” British Academy Lectures 2014-15, British Academy, 2016, https://doi.org/10.5871/bacad/9780197265987.003.0008.64. Wiserke, J., Stern, H., Igelström, K. (2018). Camouflaging of repetitive movements in autistic female and transgender adults. bioRxiv 412619; doi: https://doi.org/10.1101/412619
65. Autism Community Priorities for Suicide Prevention. An International Society for Autism Research (INSAR) Policy Brief 2021. Available online: https://cdn.ymaws.com/www.autism-insar.org/resource/resmgr/files/policybriefs/2021-insar_policy_brief.pdf (accessed on April 8, 2022)
66. Hirvikoski, T., Mittendorfer-Rutz, E., Boman, M. Larsson, H. Lichtenstein, P., Bölte, S. (2016). Premature Mortality in Autism Spectrum Disorder. Br. J. Psychiatry, 208, 232–238.
67. daVanport, S. (2019) Righting the gender imbalance in autism studies. https://www.spectrumnews.org/features/deep-dive/righting-gender-imbalance-autism-studies/
68. Ratto, A. B., Kenworthy, L., Yerys, B. E., Bascom, J., Wieckowski, A. T., White, S. W., Wallace, G. L., Pugliese, C., Schultz, R. T., Ollendick, T. H., Scarpa, A., Seese, S., Register-Brown, K., Martin, A., & Anthony, L. G. (2017). What About the Girls? Sex-Based Differences in Autistic Traits and Adaptive Skills. Journal of Autism and Developmental Disorders, 48(5), 1698–1711. https://doi.org/10.1007/s10803-017-3413-9
69. Kreiser, N.L., & White, S.W. (2014). ASD in Females: Are We Overstating the Gender Difference in Diagnosis?. Clin Child Fam Psychol Rev 17, 67–84. https://doi.org/10.1007/s10567-013-0148-9
70. Ormond, S., Brownlow, C., Garnett, M. S., Rynkiewicz, A., & Attwood, T. (2018). Profiling Autism Symptomatology: An Exploration of the Q-ASC Parental Report Scale in Capturing Sex Differences in Autism. Journal of Autism and Developmental Disorders, 48(2), 389–403. https://doi.org/10.1007/s10803-017-3324-9
71. Attwood, T., Garnett, M. S., & Rynkiewicz, A. (2011). Questionnaire for Autism Spectrum Conditions (Q-ASC) [Measurement instrument].
72. Hull, L., Mandy, W., Lai, M.-C., Baron-Cohen, S., Allison, C., Smith, P., & Petrides, K. V. (2018). Development and Validation of the Camouflaging Autistic Traits Questionnaire (CAT-Q). Journal of Autism and Developmental Disorders, 49(3), 819–833. https://doi.org/10.1007/s10803-018-3792-6
73. Clarke, E., Hull, L., Loomes, R., McCormick, C. E., Sheinkopf, S. J., & Mandy, W. (2021). Assessing gender differences in autism spectrum disorder using the Gendered Autism Behavioral Scale (GABS): An exploratory study. Research in Autism Spectrum Disorders, 88, 101844. https://doi.org/10.1016/j.rasd.2021.101844
Photo by Omar Lopez on Unsplash




